That clicking sound isn’t normal — and the pain that follows isn’t either.
Maybe it started as an occasional pop when you yawned. Or a subtle clicking while chewing. At first, more annoying than alarming. But now the clicking is constant. Your jaw feels tight. Opening your mouth wide sends sharp pain through your face. Chewing has become uncomfortable.
Ignore it, and you might end up unable to eat without pain or needing invasive jaw surgery.
What you’re experiencing is likely temporomandibular joint disorder (TMJ disorder), and it’s your body’s urgent warning that something needs attention now, before permanent damage sets in.
The good news? TMJ disorder physiotherapy can address the root causes and help you avoid surgery. But timing matters.
What Is TMJ Disorder?

The temporomandibular joint connects your lower jaw to your skull, just in front of your ears. Unlike most joints, it moves in multiple directions simultaneously — up, down, side to side, forward and backward. This complexity makes it functional but vulnerable.
When the joint disc, ligaments, muscles, or joint capsule becomes damaged or dysfunctional, you experience TMJ disorder. That clicking sound? It’s often your joint disc slipping out of position and snapping back.
The Real Causes Behind Your Jaw Pain
1. Teeth Grinding and Jaw Clenching (Bruxism)
The most common culprit. Grinding creates up to 250 pounds of pressure on your TMJ, wearing down the protective disc and straining muscles — often for hours every night while you sleep.
Signs you’re grinding:
- Worn, flattened, or chipped teeth
- Waking with jaw soreness or headaches
- Tongue or cheek indentations
- Increased tooth sensitivity
2. Poor Posture
Forward head posture from computer or phone use dramatically affects your TMJ. For every inch your head moves forward, it adds 10 pounds of pressure to your neck and changes jaw mechanics.
Your jaw gets pulled backward, the TMJ compresses, neck muscles tighten, and the entire system shifts out of alignment.
3. Stress and Tension
Psychological stress manifests physically. Subconscious jaw clenching throughout the day, increased muscle tension, and disrupted sleep all compound TMJ problems.
Check right now — are your teeth touching? If you’re not eating, they shouldn’t be.
4. Other Contributing Factors
- Direct trauma or injury to the jaw
- Malocclusion (misaligned bite)
- Missing teeth or poorly fitted dental work
- Arthritis affecting the joint
- Disc displacement inside the TMJ
Warning Signs: From Clicking to Crisis
Early Stage (Act Now!)
- Clicking or popping sounds
- Morning jaw stiffness
- Occasional discomfort
- Jaw fatigue after eating or talking
- Slight deviation when opening
Progressive Stage
- Persistent pain in jaw, ear, or temple
- Frequent headaches
- Neck and shoulder pain
- Difficulty eating certain foods
- Jaw locking temporarily
- Limited mouth opening
- Ear ringing or fullness
Advanced Stage (Don’t Let It Get Here)
- Chronic, debilitating pain
- Severe joint damage
- Inability to chew properly
- Sleep disruption
- Dental destruction
- Social and work impact
How TMJ Affects Your Whole Body
TMJ disorder doesn’t stay localized:

- Headaches and migraines from jaw muscle tension
- Neck and shoulder dysfunction from compensation
- Postural changes affecting your entire spine
- Sleep deprivation from pain and grinding
- Nutritional compromise from avoiding foods that hurt to chew
- Mental health impact from chronic pain
Why Mouth Guards Aren’t Enough
Dentists often recommend mouth guards, medication, or dental adjustments. These help but typically don’t address:
- Underlying muscle tension
- Postural dysfunction
- Movement patterns
- Stress-related clenching
- Neck and shoulder involvement
This is where jaw pain treatment through physiotherapy excels — by addressing root causes, not just symptoms.
TMJ Disorder Physiotherapy: The Complete Solution
Comprehensive Assessment
Your physiotherapist evaluates:
- Pain patterns and symptom history
- Jaw range of motion and movement quality
- Muscle tension and trigger points
- Posture from head to shoulders
- Neck mobility and alignment
- Bite patterns and compensations
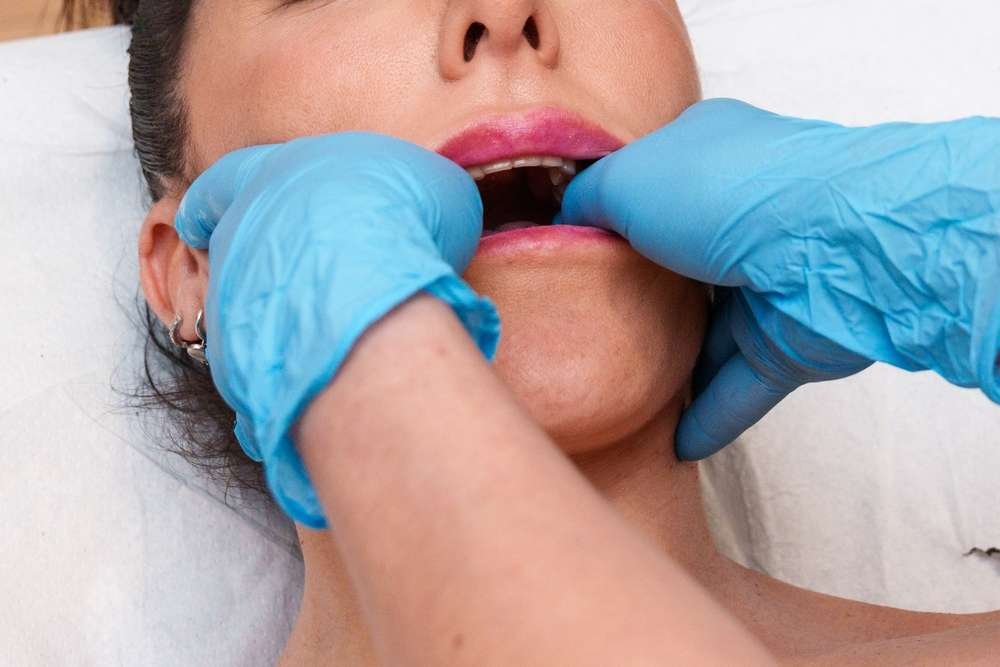
Manual Therapy Techniques
Intraoral work (inside your mouth):
- Releasing tight jaw muscles
- Direct TMJ mobilization
- Trigger point release
- Improving tissue mobility
Extraoral treatment (outside):
- Masseter and temporalis muscle release
- Facial mobilization
- Joint mobilization for better mechanics
- Neck and upper back treatment
Therapeutic Exercises
Restoring jaw function:
- Controlled opening exercises
- Strengthening without strain
- Coordination training
- Proprioceptive awareness
Supporting muscles:
- Neck strengthening for posture
- Shoulder blade stabilization
- Deep neck flexor activation
Flexibility and relaxation:
- Gentle jaw stretching
- Neck and shoulder releases
- Progressive muscle relaxation
- Breathing techniques
Postural Correction
Addressing the posture-jaw connection:
- Workstation ergonomics
- Screen and phone positioning
- Posture retraining
- Daily habit modification
Education and Self-Management
Learning to protect your TMJ:
- Recognizing and stopping clenching
- Keeping teeth apart during the day
- Avoiding jaw-straining activities
- Dietary modifications during healing
- Stress management techniques
- Optimal sleep positions
Your Recovery Timeline
Weeks 1-4: Pain Reduction
- 2-3 sessions per week
- Immediate relief from manual therapy
- Learning basics of self-care
- 30-50% pain improvement
Weeks 4-12: Function Restoration
- 1-2 sessions per week
- Progressive strengthening
- Postural corrections
- 60-80% improvement
3+ Months: Long-Term Management
- Monthly check-ins as needed
- Advanced stability work
- Sustainable self-management
- Minimal to no pain
Most patients see meaningful improvement within 6-12 weeks with consistent TMJ disorder physiotherapy.
Prevention: Protecting Your TMJ
Once recovered, maintain TMJ health through:
Daily habits:
- Check for clenching several times daily
- Practice good posture during screen time
- Take breaks every 30 minutes
- Continue 5-10 minutes of exercises
- Manage stress proactively
Ergonomics:
- Screen at eye level
- Supportive chair and desk setup
- Phone held up, not looking down
When to seek help again:
- Symptoms returning
- After dental procedures or injury
- During high-stress periods
- Any significant change in jaw function
The Cost of Waiting
Ignoring the problem:
- Years of worsening symptoms
- Thousands on ineffective treatments
- Potential surgery ($5,000-$50,000)
- Permanent joint damage
- Lost quality of life
Acting now with physiotherapy:
- 3-6 months to major improvement
- Cost-effective treatment
- Prevention of permanent damage
- Return to normal eating and living
- Avoiding surgery
Take Action Now
Your jaw has been sending signals. That clicking isn’t a quirk. That pain won’t disappear on its own. That difficulty eating will only worsen.
Your next steps:
- Schedule an evaluation with a TMJ-specialized physiotherapist
- Document your symptoms — when, where, what triggers them
- Assess your habits — clenching, posture, stress
- Commit to recovery — home exercises and lifestyle changes matter
TMJ disorder is progressive when ignored but highly treatable when addressed properly. You don’t have to live with jaw pain or avoid foods you love. You don’t have to accept dysfunction as normal.
Recovery is possible. Relief is achievable. But only if you act now.
Your jaw is asking for help. It’s time to listen.





