The room spins. You can’t walk straight. And doctors keep telling you to “wait it out.”
You wake up, turn your head, and suddenly the world tilts violently. Nausea crashes over you. Simple tasks — driving to work, walking through a store, bending down — become terrifying challenges. You’ve tried medications and waited months, yet the dizziness persists.
Living with vertigo means living in fear of falling, driving, or even standing up — but it doesn’t have to be permanent.
The dizziness you’re experiencing likely stems from treatable vestibular disorders — inner ear conditions that medication alone cannot fix. The solution? Specialized vestibular physiotherapy that can provide dramatic relief, often within just a few sessions.
Why Your Inner Ear Controls Your Balance
Your sense of balance comes from your vestibular system in your inner ear — your body’s internal gyroscope. This system includes:
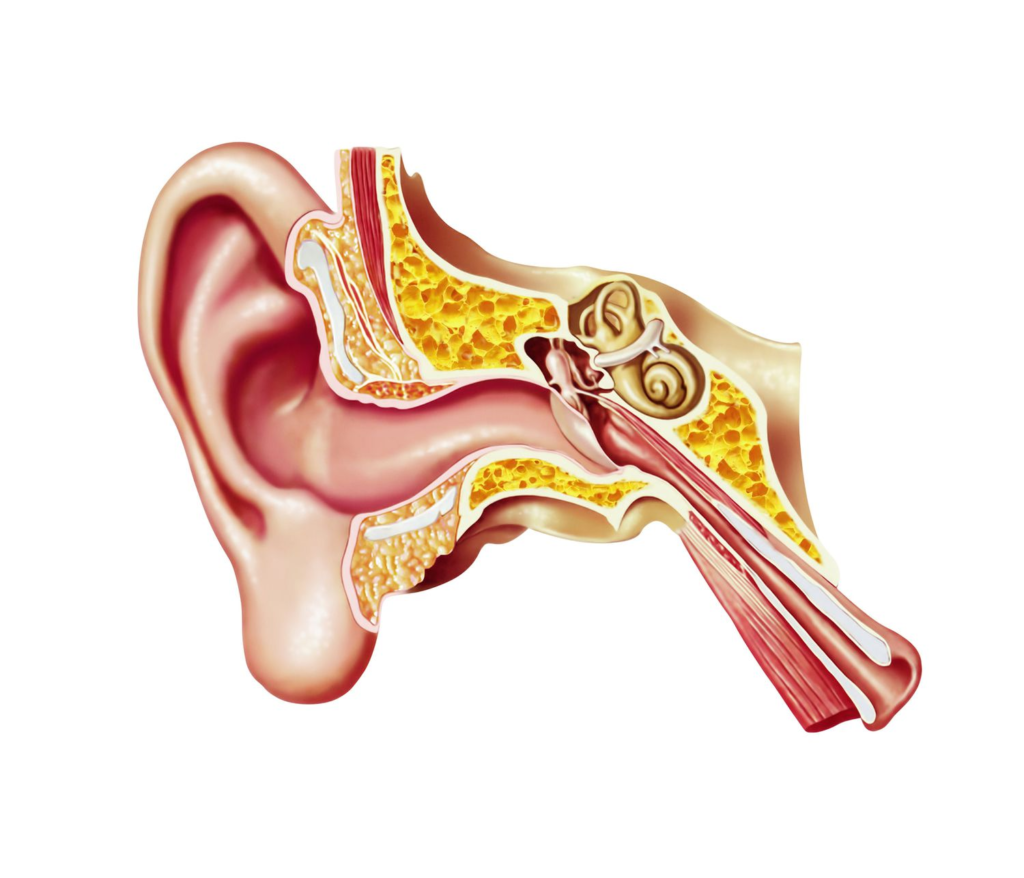
- Semicircular canals: Fluid-filled loops that detect rotational head movements
- Otolith organs: Structures with calcium crystals that sense linear motion and head position
- Vestibular nerve: Transmits balance information to your brain
Your brain integrates signals from both ears, your eyes, and muscle sensors to maintain balance. When something disrupts this system — displaced crystals, inflammation, or nerve damage — your brain receives conflicting signals, creating the disorienting sensation of vertigo.
The Most Common Vestibular Disorders
Benign Paroxysmal Positional Vertigo (BPPV)
BPPV accounts for 50% of all vertigo cases. Tiny calcium crystals dislodge and migrate into the semicircular canals. When you change position, these crystals trigger false signals that your head is spinning.
Symptoms:
- Brief episodes of intense spinning (10-60 seconds)
- Triggered by rolling over, looking up, or lying down
- Accompanied by nausea or vomiting
Why medication fails: BPPV is mechanical, not chemical. Medication can’t reposition displaced crystals.
Vestibular Neuritis and Labyrinthitis
Viral infections cause inflammation in the vestibular nerve or entire inner ear structure, disrupting balance signals.
Symptoms:
- Sudden, severe vertigo lasting days to weeks
- Significant nausea and difficulty walking
- Hearing loss and tinnitus (with labyrinthitis)
Why medication has limits: It reduces inflammation but doesn’t restore vestibular function or help your brain compensate.
Ménière’s Disease
Abnormal fluid accumulation in the inner ear creates pressure changes affecting balance and hearing.
Symptoms:
- Recurring vertigo episodes (20 minutes to hours)
- Fluctuating hearing loss in one ear
- Tinnitus and ear fullness
- Progressive hearing loss over time
Vestibular Migraine
Migraine-related brain changes affect vestibular processing, causing dizziness with or without headache.
Symptoms:
- Vertigo episodes lasting minutes to hours
- Sensitivity to motion, light, or sound
- May occur without headache
Why Traditional Treatment Falls Short
Most doctors prescribe vestibular suppressants (like meclizine) or tell you to wait. Here’s the problem:
Suppressant medications reduce symptoms by depressing vestibular activity, but this slows recovery. Your brain needs accurate signals to adapt — suppressing them interferes with healing.
Anti-nausea medications address symptoms without treating the dysfunction.
Waiting assumes spontaneous recovery, but many people develop chronic balance problems lasting months or years.
The missing piece: Traditional approaches manage symptoms rather than rehabilitate the vestibular system.
How Vestibular Physiotherapy Works
Vestibular physiotherapy uses specific exercises and maneuvers based on three principles:
1. Repositioning: Moving Crystals Back
For BPPV, canalith repositioning maneuvers use gravity to guide displaced crystals back to their proper location.

The Epley Maneuver:
- Precise sequence of head and body positions
- Each position held 30-60 seconds while crystals move
- 70-90% success rate after 1-3 sessions
- Many people experience immediate relief
2. Adaptation: Retraining Your Brain

When vestibular damage persists, your brain needs to recalibrate balance processing. Adaptation exercises repeatedly expose you to movements that trigger dizziness, gradually reducing the sensory mismatch.
Common exercises:
- Gaze stabilization: Focus on a target while moving your head to train vision stability
- Visual motion training: Watch moving patterns to desensitize your system
- Dynamic visual acuity: Read while moving your head
These exercises provoke mild symptoms initially — that’s how your brain adapts. With consistent practice (3-5 times daily), most people improve within 2-6 weeks.
3. Substitution: Alternative Balance Strategies
When vestibular function is permanently impaired, your brain learns to rely more on vision and body position sense.
Balance retraining progresses through:
- Standing with feet together or tandem, eyes open then closed
- Standing on foam surfaces
- Single-leg standing with head movements
- Walking with head turns
- Navigating obstacles and uneven surfaces
What to Expect
Assessment
A comprehensive evaluation (45-60 minutes) includes:
- Symptom history and triggers
- Eye movement observation
- Positional testing for BPPV
- Balance and gait assessment
- Functional testing
Treatment Timeline
BPPV: Immediate to near-immediate results. Most people improve after 1-3 sessions over 1-2 weeks.
Vestibular neuritis/labyrinthitis: 4-8 weeks with 1-2 sessions weekly plus daily home exercises.
Chronic vestibular disorders: 8-12+ weeks depending on severity.
Home Exercises Are Essential
Success depends on performing exercises 3-5 times daily. The temporary increase in symptoms during exercises signals your brain is adapting — exactly what needs to happen for recovery.
The Research Evidence
BPPV: Repositioning maneuvers are significantly more effective than medication or waiting. For every three people treated, two experience complete resolution.
Vestibular neuritis: Early rehabilitation leads to faster, more complete recovery than medication alone.
Chronic dizziness: 80-85% of people experience significant improvement with vestibular rehabilitation.
Fall prevention: Treatment reduces fall risk by improving balance reactions and confidence.
When to Seek Help
Consider vestibular physiotherapy if you have:
- Vertigo triggered by head movements
- Chronic dizziness lasting more than a few days
- Balance problems or unsteadiness
- Dizziness that hasn’t responded to medication
- Fear of falling or needing support when walking
- Difficulty focusing during head movement
- Sensitivity to busy visual environments
Seek emergency care for:
- First-time severe vertigo with headache or confusion
- Vertigo with chest pain or irregular heartbeat
- Sudden hearing loss
- Vertigo with slurred speech or weakness
Finding a Qualified Therapist
Look for physiotherapists with:
- Certification in vestibular rehabilitation
- Experience treating vertigo and balance disorders
- Appropriate assessment tools
Ask: “How many vestibular patients do you treat monthly?” and “What’s your success rate with BPPV?”
Your Action Plan
Today:
- Document your symptoms: triggers, duration, frequency
- Research vestibular physiotherapists in your area
This Week:
- Schedule an assessment
- Prepare to describe symptoms in detail
- Bring medication lists and test results
During Treatment:
- Commit to daily home exercises
- Track your progress
- Communicate openly with your therapist
- Be patient with gradual improvement
Stop Waiting, Start Recovering
That spinning sensation and constant unsteadiness aren’t normal aging or something you must accept. They’re symptoms of treatable vestibular disorders that respond remarkably well to specialized physiotherapy.
Medication masks symptoms temporarily but won’t fix the underlying problem. Waiting rarely leads to resolution. Only targeted vestibular rehabilitation addresses the root cause, retrains your balance system, and restores your quality of life.
For BPPV sufferers, relief often comes within a single session. For other conditions, consistent treatment over weeks produces dramatic improvements in balance, confidence, and independence.
The room doesn’t have to keep spinning. You can walk straight. And you definitely don’t have to “wait it out.”
Your balance and independence are within reach. The first step is scheduling that initial assessment. Make the call today — the relief you’ve been seeking may be just one appointment away.
Ready to regain your balance and confidence? Contact a certified vestibular physiotherapist today for a comprehensive assessment. Your path to stability starts now.





